Age-Related Macular Degeneration (ARMD)
Help for Age-Related Macular Degeneration in Wilmington

What Is Age-Related Macular Degeneration?
Age-related macular degeneration (ARMD) is the leading cause of vision loss in older American adults, and the most common reason patients are referred to Cape Fear Retinal Associates for further evaluation, treatment and care. Patients afflicted with ARMD may note a worsening of their central vision while retaining good peripheral vision.
Many patients with macular degeneration share a common misconception and fear that the disease will automatically progress to blindness. As suggested by its name, ARMD only affects the macula. The macula is the central part of the retina responsible for detailed visual tasks. In macular degeneration, patients suffer varying degrees of destruction to this tissue and can experience a wide spectrum of visual problems. These include, but are not limited to, blurred central vision, increasing difficulty with reading, patchy visual loss, and the distortion or warping of straight objects. However, even patients with advanced macular disease tend to retain excellent peripheral vision.
Who Is at Risk for Developing Macular Degeneration?
Macular degeneration primarily affects older Caucasian individuals, although cases have been reported in younger patients and those not of Caucasian descent. Additionally, a number of risk factors predispose certain people to the development and progression of the disease, including:
- Hypertension (high blood pressure)
- Cigarette smoking
- Ultraviolet light exposure
- Nutrition
- Having a family member with ARMD
Regarding the last risk factor, much research has been done regarding the genetics of macular degeneration. Although there is currently no way to definitively predict who will or will not develop ARMD, those with affected relatives are at significantly higher risk. As a result, adult relatives of ARMD patients should schedule an appointment with a retinal specialist and undergo a baseline evaluation and dilated exam.
Is There More Than One Kind of Macular Degeneration?
Generally, patients with ARMD are grouped into one of two categories:
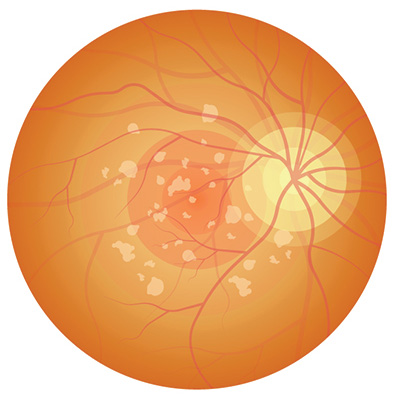
“Dry” Age-Related Macular Degeneration
The most common form of macular degeneration is caused by aging and thinning of the tissues of the macula. Dry ARMD is characterized by thinning of the macula and gradual deterioration of vision. It develops slowly and usually causes mild vision loss. As this form of the disease develops, people often notice a dimming of vision while reading.
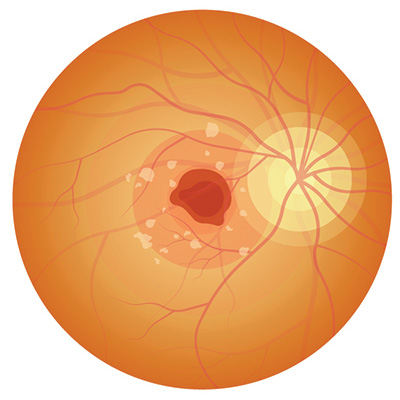
“Wet” Age-Related Macular Degeneration
Wet ARMD is so called because it is marked by an accumulation of fluid underneath the retina. In contrast with dry macular degeneration, patients with wet ARMD often, but not always, experience sudden and severe visual losses.
Symptoms include:
- A dark area or a “white-out” appears in the center of vision
- Blurred or fuzzy vision
- Color perception fades or changes
- Straight lines, such as sentences on a page or telephone poles, appear wavy or distorted
What Tests Are Helpful in Aiding Diagnosis?
Dry and wet macular degeneration impact vision in different ways, and are also treated quite differently. Sometimes it is difficult to differentiate between dry and wet ARMD, so our retinal specialists will use a variety of clinical tests and exam techniques to make an accurate diagnosis.
During an initial visit for macular degeneration, patients typically undergo two tests: fluorescein angiography (FA) and optical coherence tomography (OCT). These tests may even be performed prior to consulting with your retinal specialist. Fluorescein angiography (FA) is considered the “gold standard” for differentiating between dry and wet ARMD. It involves the injection of a small amount of vegetable-based dye through a patient’s peripheral vein – usually the arm or hand. Shortly afterward, a certified ophthalmic angiographer will take a series of time-dependent retinal photographs. The injected dye lights up the retina’s intricate vascular network and helps our specialists pinpoint a precise area of leakage in those patients with wet macular degeneration. Not only is this useful in determining the extent and progression of the disease, but it also helps when targeting specific treatment zones with specialized laser therapy.
Optical coherence tomography (OCT) is a noninvasive, quick exam that has gained universal acceptance during the last decade and is now used by many ophthalmologists. Using reflected light rays, OCT provides a detailed, highly magnified, cross-section view of a patient’s macula. Sometimes, it will uncover tiny areas of leakage not readily apparent to a retina specialist during a microscopic exam.
Patients Play an Important Role in Diagnosis & Care
Despite recent advances in ophthalmic imaging, there is no single test that can be relied upon to direct treatment and clinical decision-making. A patient’s relationship with their retinal specialist is at the core of our practice philosophy, and good patient-physician communication is critical. When making important decisions about retinal health, it is very much a joint effort. The patient’s perception of his or her visual health and the patient’s perception of any vision changes, however slight, are every bit as important in directing care as are the clinical tests.
As a result, every patient diagnosed with macular degeneration should establish a daily routine for monitoring their own vision. This is most simply and reliably performed with an Amsler grid, a simple patchwork of straight vertical and horizontal lines. We are happy to provide one to you at no cost – simply ask one of our nurses.
Amsler Grid
The Amsler grid may be helpful in revealing signs of wet age-related macular degeneration (AMD). It is not a substitute for regularly scheduled eye exams and testing.
Directions
- Do not remove glasses or contacts you normally wear for reading.
- Stand approximately 13 inches (33 cm) from the grid in a well-lighted room.
- Cover one eye with your hand and focus only on the center dot with your uncovered eye. Repeat with the other eye.
- If you see wavy, broken or distorted lines, blurred or missing areas of vision, you may be displaying symptoms of AMD and should contact your eye care provider immediately.
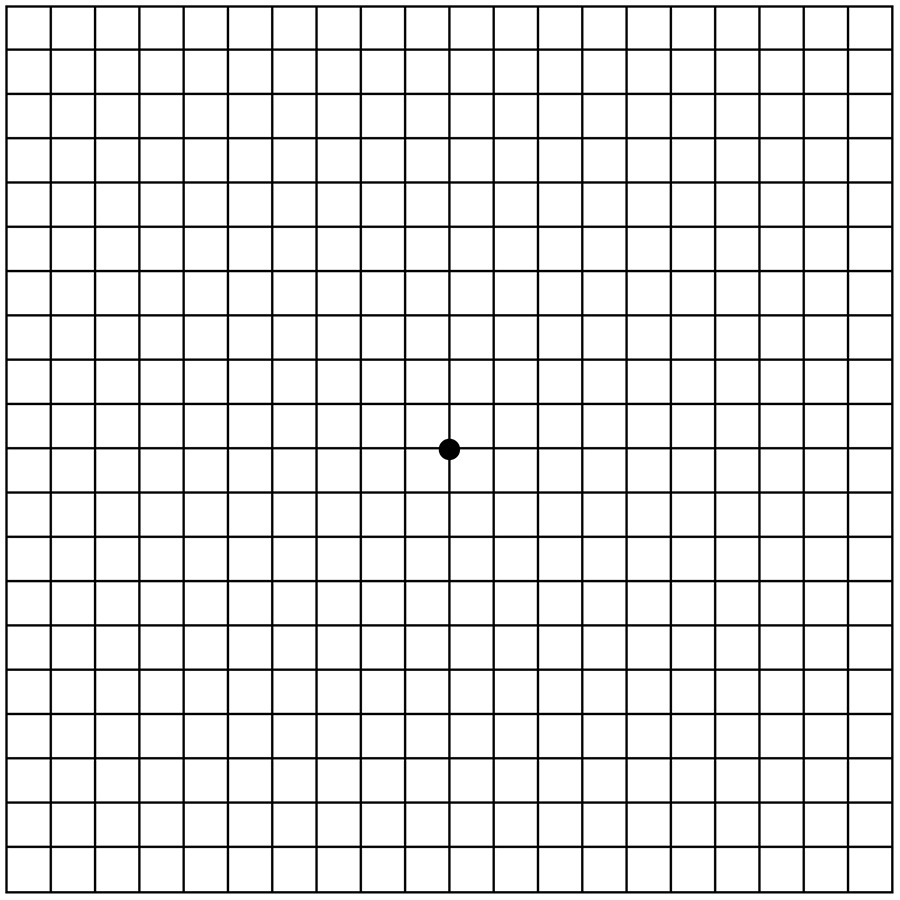
Often, patients with subtle progression of macular disease will report new “waviness” or “missing areas” when monitoring their grid. Should you or a family member notice new changes on an Amsler grid, contact us promptly. Either your retinal specialist or one of their trained ophthalmic nurses are always available to consult with you by phone. As a general rule, patients who receive treatment in a more timely fashion tend to fare better than those who delay evaluation by a retinal specialist.
What Treatments Are Available?
Medical researchers have thrown themselves fully into the battle against macular degeneration, and dramatic progress has been made in the effort to combat age-related vision loss. The most effective treatments are Avastin™, Lucentis™ and Eylea™, which help block certain growth factors that are thought to cause “leaky” blood vessel growth in wet macular degeneration. Both of these medications are introduced directly into the eye through a tiny needle. While the thought of an “eye shot” might cause many to cringe, in our experience, there is little, if any, patient discomfort, and the spectacular visual gains far outweigh any fears. Avastin™, Lucentis™ and Eylea™ are the first medicines that have actually improved vision for many patients with wet macular degeneration. Your doctor will discuss the medication that he believes will be the most effective in your situation. While they have received much media attention and deserved fanfare for their impact on wet ARMD, invaluable work continues on the dry ARMD front as well. A number of vitamin therapies are already available to slow the progression of dry ARMD, and our physicians are currently prescribing medications based on the results of the second-generation vitamin study that will hopefully prove even more beneficial than previously prescribed supplement regimens.
Low Vision Rehabilitation
This can help people who have experienced mild to severe vision loss adjust to their condition and continue to enjoy active and independent lifestyles. Low vision rehabilitation may involve anything from adjusting the lighting in your home to learning to use low vision aids to help you read and perform daily tasks. Our retinal specialists can refer patients to local low vision specialists for this assistance.

